What is the MCL? Where is the MCL located?
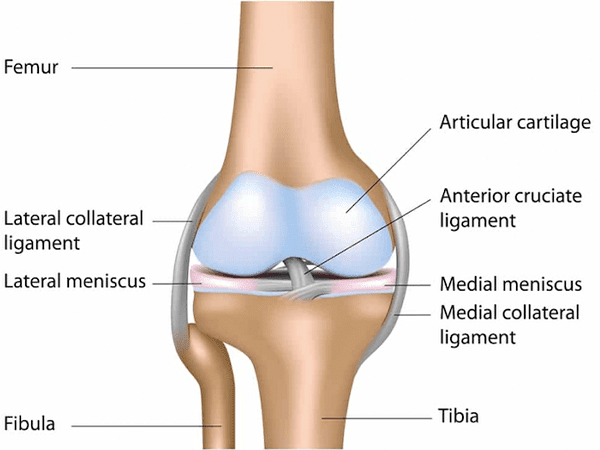
The MCL, or medial collateral ligament, is a vital ligament in the human body that provides stability to the knee joint. It is located on the inner side of the knee and connects the femur (Thigh bone) to the tibia (Shin bone). The MCL helps prevent excessive inward movement or valgus stress to the knee, protecting it from injury. It plays a crucial role in maintaining knee stability during activities such as walking, running, and changing directions.
What is the Posteromedial corner of the knee?
The Posteromedial corner of the knee refers to the complex network of structures located at the back and inner side of the knee joint. It consists of several ligaments, tendons, muscles, and other soft tissues that provide stability and support to the knee. These structures include the posterior oblique ligament, the posterior capsule, the medial collateral ligament, the semimembranosus tendon, the Posteromedial joint capsule, and other surrounding tissues. The Posteromedial corner plays a crucial role in maintaining the stability and function of the knee, particularly during rotational movements and valgus stress.
How does the Posteromedial corner work?
The Posteromedial corner of the knee works by providing stability and support to the joint during rotational movements and valgus stress. It consists of ligaments, tendons, and muscles that work together to resist excessive inward movement and rotational forces. The ligaments and soft tissues in the Posteromedial corner help control the motion of the knee, preventing excessive laxity and maintaining proper alignment. This stability is essential for maintaining the overall function and integrity of the knee joint.
How do Posteromedial corner injuries occur?
Posteromedial corner injuries of the knee can occur due to various reasons. They are commonly caused by high-energy trauma, such as sports-related collisions, motor vehicle accidents, or falls. The injuries can involve ligament tears, tendon avulsions, or fractures. Sudden and forceful twisting or hyperextension of the knee joint can also lead to Posteromedial corner injuries. These injuries require appropriate diagnosis and treatment to restore knee stability and function.
What are the symptoms of an MCL tear?
Symptoms of an MCL tear typically include pain and tenderness along the inner side of the knee.
Swelling and stiffness may also be present, along with a feeling of instability or giving way in the knee.
Range of motion may be limited, and there may be difficulty bearing weight on the affected leg. Some individuals may experience a popping or snapping sensation at the time of injury.
Do Posteromedial corner injuries of the knee heal on their own?
Posteromedial corner injuries of the knee generally do not heal on their own. These injuries often require medical intervention for proper healing. Treatment options may include conservative measures like rest, physical therapy, and bracing, or in more severe cases, surgical repair or reconstruction. It is important to seek medical evaluation and follow the recommended treatment plan to optimize healing and restore knee stability and function.
What is the most accurate way to diagnose a Posteromedial corner injury?
The most accurate way to diagnose a Posteromedial corner injury is through a combination of clinical evaluation, imaging studies, and specialized tests. A thorough physical examination by a healthcare professional can assess knee stability, range of motion, and identify specific signs of the injury. Diagnostic imaging, such as MRI or X-ray, can provide detailed visualization of the structures involved.
Additionally, specific tests like stress radiographs or dynamic ultrasound may be performed to evaluate ligament laxity and confirm the diagnosis.
What is the best time to fix a Posteromedial corner injury?
The optimal timing for fixing a Posteromedial corner injury depends on several factors, including the specific injury, associated injuries, and the overall condition of the knee. In general, it is often
recommended to address these injuries sooner rather than later to prevent complications and promote optimal healing. However, the timing of surgical intervention should be determined on an individual basis, taking into account factors such as the extent of injury, patient’s overall health, and surgeon’s recommendation.
How is the Posteromedial corner fixed?
The treatment approach for fixing a Posteromedial corner injury depends on the severity and specific structures involved. Surgical intervention is often required to restore stability and function. The procedure typically involves repairing or reconstructing damaged ligaments and tendons using various techniques, such as sutures, anchors, or grafts. The surgeon may also address any associated fractures or bony abnormalities. Rehabilitation and physical therapy play a crucial role in the post-operative period to optimize recovery and regain knee strength and mobility.
How long is the recovery?
The recovery period for a Posteromedial corner injury can vary depending on the severity of the injury, the surgical procedure performed, and individual factors. In general, the initial phase of recovery involves immobilization, followed by a progressive rehabilitation program. It may take several weeks to months to regain full strength, range of motion, and return to normal activities. The specific timeline and milestones of recovery should be discussed with the treating physician or surgeon.
MCL Tears Posteromedial
Treatment options for MCL tears can include both conservative and surgical approaches. Conservative
treatment involves rest, ice, compression, and elevation (RICE), along with bracing and physical therapy
to strengthen the surrounding muscles and support the healing process. In more severe cases or when
conservative measures fail, surgical intervention may be considered, which can involve MCL repair or
reconstruction using sutures or grafts. The treatment approach depends on the severity and individual
circumstances and should be discussed with a healthcare professional.
Types of Posteromedial
MCL injuries can be classified into three types based on severity: Grade 1, Grade 2, and Grade 3. Grade 1
MCL injuries involve minor stretching or microscopic tears of the ligament, resulting in mild pain and
tenderness but without significant instability. Grade 2 injuries involve a partial tear of the ligament,
causing moderate pain, swelling, and some joint instability. Grade 3 injuries are complete tears of the
ligament, leading to severe pain, swelling, and significant joint instability